What Is Bioindividualized Medicine?

Bioindividualized medicine is a patient-centered approach that recognizes the uniqueness of each person's biology, genetics, and environmental interactions. Unlike conventional medicine, which often relies on standardized treatments, bioindividualized care focuses on tailoring interventions to a person’s specific physiological and genetic profile. This method seeks to address the root causes of health issues rather than simply alleviating symptoms.
Acknowledging the fact that an equal reaction to the same therapy could not be demonstrated in two humans is the foundation of this concept. Attempts at personalized care require considerations of such factors as genetic profile, metabolism, balance of the microbiome, insufficiency of key nutrients, levels of exposure to possible toxins, and the lifestyle of the patient. The integration of these factors by the practitioner offers a platform for the development of safer, more effective, and more sustainable interventions.
Key Principles of Bioindividualized Medicine
- Patient-Centered Care: Treatment plans are tailored to individual biological, genetic, and lifestyle needs.
- Root Cause Focus: Strategies target underlying dysfunctions rather than just symptoms.
- Integrative Approach: Combines conventional medicine with nutritional, lifestyle, and complementary therapies.
- Preventive Focus: Emphasizes early intervention and personalized prevention strategies.
Bioindividualized medicine does not reject conventional medicine but integrates it within a broader framework that considers each person’s unique biology. It often involves collaboration between multiple health disciplines to provide a holistic and personalized care plan.
Genetic Polymorphisms and Their Impact on Health
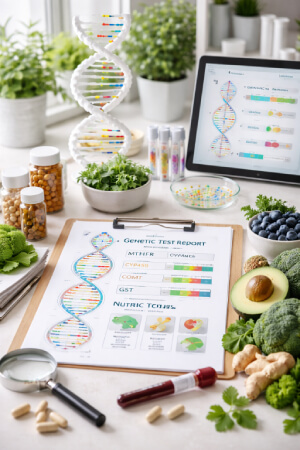
Genetic polymorphisms are variations in DNA sequences among individuals. These differences can significantly influence how the body metabolizes nutrients, responds to medications, or handles environmental exposures. Understanding genetic polymorphisms allows practitioners to anticipate potential health risks and tailor interventions more accurately.
Gene variation affecting detoxification pathways, like the GSTM1 or CYP450 enzymes, can influence the metabolization of various toxins and medicines most efficiently. Additionally, gene polymorphisms related to nutrient metabolism - for instance the MTHFR are believed to modulate folate metabolism and increase the chances of chronic conditions. By detecting such genetic traits, the specialists can give dietary plans, supplements, or therapeutic interventions to all those concerned in improving health outcomes.
Common Genetic Variations in Personalized Medicine
- MTHFR Polymorphisms: Influence folate metabolism and cardiovascular health.
- CYP450 Variants: Affect drug metabolism, potentially altering efficacy and side effects.
- COMT Variations: Impact neurotransmitter breakdown and stress response.
- GST Enzyme Variants: Influence detoxification and susceptibility to environmental toxins.
These genetic insights are not deterministic but provide valuable guidance for preventive strategies, nutrition, lifestyle adjustments, and treatment planning. By combining genetic information with functional assessments, practitioners can develop highly targeted health interventions.
How Genetics Guides Integrative Health Plans
Genetic testing in bioindividualized medicine is typically used to identify potential vulnerabilities and strengths in an individual’s metabolism, detoxification, and nutrient requirements. This information allows for:
- Personalized Nutrition: Adjusting macronutrient ratios and micronutrient supplementation.
- Medication Optimization: Choosing medications or dosages based on predicted metabolic response.
- Lifestyle Customization: Tailoring exercise, sleep, and stress management approaches.
Integrating genetic information into health planning ensures that interventions are not only effective but also minimize potential adverse effects, enhancing long-term well-being.
Integrative Health Approaches in Personalized Medicine
A patient is the perfect example of a person who gives back to the community. Integrative health is the combination of conventional treatment with complementary therapies based on evidence. This is done to create a holistic personalized plan for individuals to address many health aspects: physical, mental, and emotional. Through this approach, we recognize the numerous interplays between genetics, lifestyle, and environmental factors, all of which contribute significantly to symptomatology.
With stimulating integrative therapies such as functional medicine, nutrition therapy, mind-body practices, etc., relief to the patient from punishing conventional practices often comes. For example, changes in diet may ameliorate genetic weaknesses, with an ordinary reduced-stress-laden lifestyle dumping the expression of potential harmful genes while promoting resilience. An understanding of integrative health between the medical modality and the patient empowers individuals to participate positively, to better understand and foster their own personal health journey.
Core Components of Integrative Health
- Nutrition and Functional Medicine: Targeted dietary interventions and nutrient optimization based on individual metabolic needs.
- Mind-Body Therapies: Techniques such as meditation, yoga, and biofeedback to reduce stress and support emotional well-being.
- Lifestyle Medicine: Personalized exercise, sleep optimization, and environmental adjustments.
- Complementary Therapies: Acupuncture, massage, and herbal medicine, integrated with conventional treatments when evidence supports efficacy.
These components work synergistically to enhance resilience, prevent disease, and support recovery. By addressing the whole person rather than isolated symptoms, integrative approaches can improve both physical and mental health outcomes.
Benefits of Integrative, Bioindividualized Care
- Improved Symptom Management: Customized interventions often lead to more effective symptom relief.
- Enhanced Prevention: Personalized plans identify and mitigate health risks before they manifest.
- Optimized Treatment Response: Understanding genetic and metabolic variations allows for safer and more effective therapy.
- Holistic Support: Addresses physical, mental, and emotional health simultaneously, improving quality of life.
The integration of genetics, nutrition, lifestyle, and complementary therapies creates a flexible framework that can adapt to changing health needs over time.
Implementing a Personalized Health Strategy

Developing a bioindividualized health plan begs the modeling of thorough assessments with a medical history, lifestyle evaluation, and appropriate genetic testing. This information allows us to spot risk factors, likely nutrient deficiencies, and possible genetic weaknesses. Following these diagnoses, specific plans are developed and packed with evidence-based walls across the platforms.
Steps to Develop a Bioindividualized Plan
- Comprehensive Assessment: Evaluate medical history, lifestyle, and potential genetic factors.
- Personalized Intervention Design: Develop nutrition, lifestyle, and therapeutic strategies based on findings.
- Implementation and Monitoring: Track results, adjust interventions, and optimize outcomes.
- Ongoing Education: Equip patients with knowledge and tools to maintain long-term health.
This stepwise approach allows individuals to experience measurable improvements while minimizing unnecessary treatments or risks.
Personalized Health for Every Individual
In bio-individualized medicine, the medical paradigm shifts to consider practices that address all the individual personal genetics on programming, including biological processes and the particularities of lifestyle in order to intuitively manage their health. American Medical Association understands genetic polymorphisms and integrative approaches such that doctors can provide highly customized personalized disturbance to allow health to flourish for the patient and prevent disease while supporting wellness.
Can genetic testing optimise psychiatric prescribing?
— Psychiatry Excellence (@psycheureka) March 21, 2025
Response to psychotropics is highly variable. Genetic polymorphisms in drug-metabolising enzymes influence efficacy, side effects, and treatment adherence.
Pharmacogenomics is reshaping psychiatry by guiding precision… pic.twitter.com/ockbZBhmLx
Best UK Casinos not on Gamstop
MTHFR polymorphisms that can lead to elevated homocysteine can be a risk factor for later fibrosis. pic.twitter.com/ykAHaYCzde
— Peter D'Adamo (@peterdadamo) December 29, 2025
Ways to manage stress!!
— SunlaCommunity (@SunlaCommunity) June 14, 2025
Regular exercise, a healthy diet, sufficient sleep, and mindfulness practice are the key to reducing stress level. pic.twitter.com/PLeMPxKqZ9
